Understanding Diabetes
Diabetes is a chronic condition that affects millions worldwide, characterized by the body’s inability to effectively process sugar. Understanding the types of diabetes is crucial for effective management. Type 1 diabetes, an autoimmune condition, requires insulin therapy due to the body’s lack of insulin production. On the other hand, Type 2 diabetes often develops later in life and is associated with lifestyle factors. This type can often be managed with lifestyle changes and medication. Additionally, gestational diabetes occurs during pregnancy and usually resolves after childbirth, though it increases the risk of developing Type 2 diabetes later in life. Educating oneself about these variations is the first step in managing diabetes effectively.
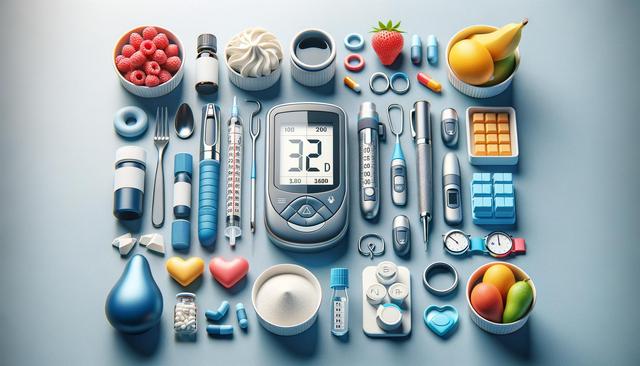
Monitoring Blood Sugar Levels
Regular monitoring of blood sugar levels is a cornerstone of diabetes management. For those with diabetes, keeping track of these levels helps in adjusting treatments and ensuring that they maintain target ranges. There are several methods available, including:
- Traditional glucometers, which require a small blood sample
- Continuous glucose monitors (CGMs), offering real-time glucose level updates
- Flash glucose monitors, allowing intermittent scanning for glucose levels
Choosing the right monitoring device depends on personal preferences and lifestyle. Regular monitoring aids in recognizing patterns and making informed decisions about diet and physical activity.
Diet and Nutrition
A balanced diet plays a crucial role in diabetes management. It is essential to focus on foods that help maintain stable blood sugar levels. Here are some dietary considerations:
- Incorporate high-fiber foods like vegetables, fruits, and whole grains
- Choose lean proteins, including fish, poultry, and plant-based options
- Limit intake of sugars and refined carbohydrates
- Stay hydrated and opt for water over sugary drinks
Meal planning can be effective in managing diabetes. Consulting a dietitian can provide personalized meal plans that align with individual health goals.
Exercise and Physical Activity
Physical activity is beneficial for everyone but holds particular significance for those managing diabetes. Regular exercise can help regulate blood sugar levels, improve cardiovascular health, and promote weight loss. Engaging in activities such as walking, cycling, or swimming is highly recommended. It’s important to:
- Set realistic exercise goals
- Incorporate a mix of aerobic activities and strength training
- Understand the effects of various exercises on blood sugar levels
- Stay consistent with a workout routine
Consulting with healthcare providers before starting any new exercise regimen is advisable, especially for those who have other health concerns.
Medication and Insulin Therapy
For many individuals, medication is an integral part of diabetes treatment. Various oral medications can help manage blood sugar levels by influencing insulin production or absorption. For those requiring insulin therapy, understanding the types of insulin and their applications is essential. Insulin can be short-acting, intermediate, or long-acting, each serving specific purposes. It’s important to:
- Follow prescribed medication plans
- Regularly consult with healthcare professionals for medication adjustments
- Stay informed about new treatment options
- Understand potential side effects and how to address them
Adhering to a medication regimen can significantly improve diabetes management and quality of life.
Conclusion
Diabetes management is a multifaceted approach that involves lifestyle changes, regular monitoring, and adherence to treatment plans. By understanding the condition and adopting a proactive attitude, individuals can live fulfilling lives while effectively managing their diabetes. It’s essential to stay informed, seek support, and regularly consult healthcare professionals to ensure the best possible outcomes.