Understanding Arthritis: A Common Yet Complex Condition
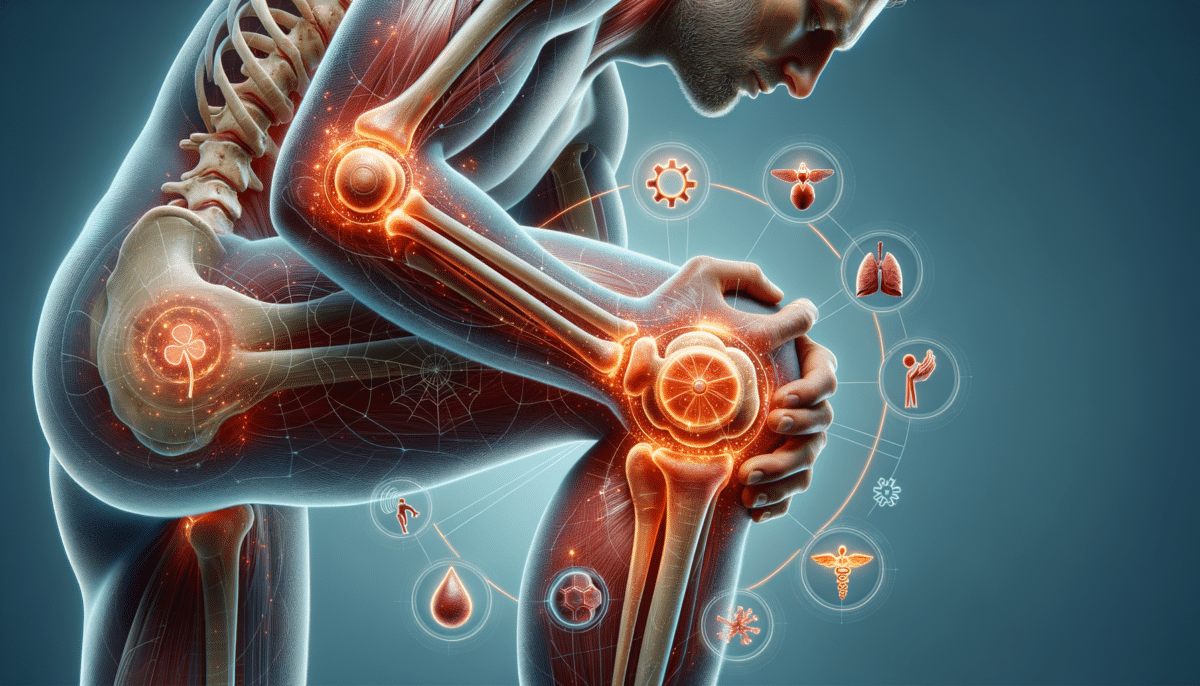
Arthritis is a prevalent condition that impacts millions of people globally, yet its complexity is often underestimated. This ailment encompasses over 100 different types, each with its own set of symptoms, causes, and treatment options. The most common forms include osteoarthritis, rheumatoid arthritis, and gout, each affecting the joints in different ways. Osteoarthritis is typically associated with the wear and tear of cartilage, while rheumatoid arthritis is an autoimmune disorder that targets the joint lining. Gout, on the other hand, results from the accumulation of uric acid crystals in the joints.
Understanding arthritis requires a multi-faceted approach, as it not only involves the physical deterioration of joints but also the emotional and social challenges that accompany chronic pain. Patients often experience stiffness, swelling, and decreased range of motion, which can significantly impact their quality of life. Moreover, the emotional toll of living with a chronic condition can lead to anxiety and depression, further complicating the management of arthritis.
Recognizing the early signs of arthritis is crucial for timely intervention. Symptoms such as joint pain, tenderness, and stiffness, especially in the morning or after periods of inactivity, should not be ignored. Early diagnosis and treatment can slow the progression of the disease and improve long-term outcomes. It’s essential for individuals to be aware of these subtle signs and seek medical advice if they suspect they may be developing arthritis.
Causes and Risk Factors: What Triggers Arthritis?
The causes of arthritis are as varied as its types, with a combination of genetic, environmental, and lifestyle factors playing a role. Genetics can predispose individuals to certain types of arthritis, such as rheumatoid arthritis and ankylosing spondylitis. However, environmental factors, including infections and physical injuries, can also trigger the onset of arthritis.
Age is a significant risk factor, as the likelihood of developing arthritis increases with age. This is particularly true for osteoarthritis, which is commonly seen in older adults due to the natural wear and tear of joints over time. Gender also plays a role, with women being more susceptible to rheumatoid arthritis, while men are more prone to gout.
Additionally, lifestyle choices can significantly impact the risk of developing arthritis. Obesity is a major risk factor, as excess weight places additional stress on weight-bearing joints, accelerating the wear and tear process. Poor diet and lack of physical activity can further exacerbate the risk. On the other hand, maintaining a healthy weight, eating a balanced diet rich in anti-inflammatory foods, and engaging in regular exercise can help reduce the risk of arthritis.
Understanding these risk factors allows individuals to make informed lifestyle choices that may prevent or delay the onset of arthritis. By adopting healthy habits and staying vigilant about joint health, individuals can take proactive steps toward managing their arthritis risk.
Symptoms and Diagnosis: Identifying Arthritis Early
Identifying arthritis early is key to managing the condition effectively, and understanding its symptoms is the first step. Common symptoms include joint pain, stiffness, swelling, redness, and decreased range of motion. These symptoms may vary in intensity and duration, often worsening with activity and improving with rest.
In addition to physical symptoms, arthritis can also manifest as fatigue, fever, and weight loss, particularly in autoimmune forms like rheumatoid arthritis. These systemic symptoms can complicate the diagnosis, as they may mimic other conditions. Therefore, it’s crucial for individuals to pay attention to persistent joint discomfort and seek medical evaluation if symptoms persist.
The diagnosis of arthritis typically involves a combination of medical history, physical examination, and diagnostic tests. Blood tests can help identify markers of inflammation and specific antibodies associated with autoimmune arthritis. Imaging techniques such as X-rays, MRI, and ultrasound are used to assess joint damage and rule out other conditions.
Early diagnosis is essential for effective management, as it allows for timely intervention and the implementation of treatment strategies to slow disease progression. By recognizing the signs of arthritis and seeking medical attention, individuals can improve their quality of life and reduce the impact of this chronic condition.
Treatment Options: Managing Arthritis Effectively
While there is no cure for arthritis, a variety of treatment options are available to manage symptoms and improve quality of life. Treatment plans are typically tailored to the individual’s specific type of arthritis, severity of symptoms, and overall health.
Medications are a cornerstone of arthritis management, with options ranging from over-the-counter pain relievers to prescription drugs. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce pain and inflammation. For more severe cases, disease-modifying antirheumatic drugs (DMARDs) and biologics may be prescribed to slow disease progression and prevent joint damage.
In addition to medication, lifestyle modifications play a crucial role in managing arthritis. Regular exercise, particularly low-impact activities like swimming and cycling, can help maintain joint flexibility and reduce stiffness. A balanced diet rich in omega-3 fatty acids, antioxidants, and anti-inflammatory foods can also support joint health.
Physical therapy and occupational therapy are valuable components of arthritis treatment, providing individuals with exercises and techniques to improve joint function and manage daily activities. In some cases, surgical interventions such as joint replacement or arthroscopy may be necessary to alleviate pain and restore mobility.
By exploring and combining various treatment options, individuals can effectively manage their arthritis symptoms and enhance their overall well-being. Collaboration with healthcare professionals is essential to develop a comprehensive treatment plan that addresses the unique needs of each patient.
Living with Arthritis: Tips for Coping and Thriving
Living with arthritis can be challenging, but with the right strategies and mindset, individuals can lead fulfilling lives. One of the most important aspects of coping with arthritis is staying informed about the condition and actively participating in one’s own care.
Education is empowering, and understanding the nature of arthritis, its triggers, and management options can help individuals make informed decisions about their health. Joining support groups or online communities can provide valuable insights and encouragement from others who share similar experiences.
Adopting a positive attitude and focusing on what can be controlled is crucial for maintaining mental and emotional well-being. Practicing mindfulness, meditation, and relaxation techniques can help manage stress and reduce the emotional burden of living with a chronic condition.
Practical tips for daily living include:
- Using assistive devices to reduce strain on joints
- Modifying workspaces to accommodate joint limitations
- Pacing activities to prevent overexertion
- Prioritizing rest and quality sleep
By implementing these strategies and maintaining open communication with healthcare providers, individuals with arthritis can navigate the challenges of their condition and continue to pursue their passions and goals. Thriving with arthritis is possible, and with the right support and resources, individuals can achieve a balanced and fulfilling life.