Understanding Ulcerative Colitis
Ulcerative colitis, commonly referred to as UC, is a significant health condition that affects a considerable number of people worldwide. As a type of inflammatory bowel disease, it primarily targets the colon, leading to chronic inflammation and ulcers in the digestive tract. The exact cause of UC ulcerative colitis remains unclear, although genetic factors, immune system malfunctions, and environmental triggers are suspected contributors. Due to the unpredictable nature of the disease, symptoms can vary greatly among individuals, and may include persistent diarrhea, abdominal discomfort, and rectal bleeding. These symptoms can significantly impact the quality of life, making management and treatment essential components of living with UC.
Symptoms and Diagnosis
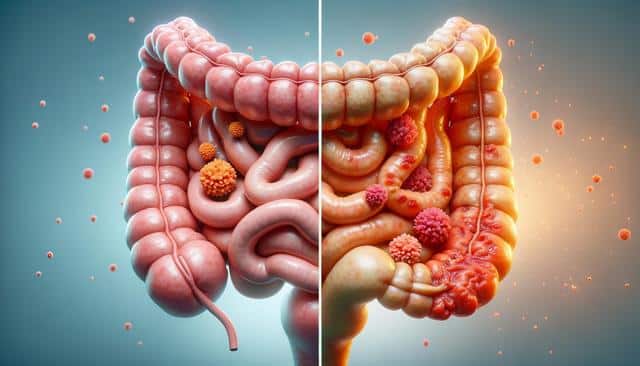
Recognizing the symptoms of UC ulcerative colitis is crucial for early diagnosis and intervention. Common symptoms include frequent episodes of diarrhea, which may be accompanied by blood or pus, abdominal pain and cramping, and the urgent need to defecate. Some individuals may also experience fever, fatigue, and weight loss. Diagnosing UC typically involves a combination of medical history evaluation, physical examinations, and a series of tests. These tests may include blood tests, stool samples, colonoscopy, and imaging studies such as CT scans. Early diagnosis is pivotal in managing the disease effectively and preventing complications such as severe dehydration, colon perforation, and increased risk of colon cancer.
Treatment Options
Managing UC ulcerative colitis often requires a multi-faceted approach. Treatment strategies are generally tailored to the individual, depending on the severity of the condition and the specific symptoms experienced. Medications play a central role in controlling inflammation and alleviating symptoms. These may include:
- Anti-inflammatory drugs like aminosalicylates and corticosteroids.
- Immunosuppressants to reduce immune system activity.
- Biologics that target specific pathways in the inflammatory response.
In addition to medication, dietary changes can also be beneficial. Identifying and avoiding foods that trigger symptoms, maintaining a balanced diet, and ensuring adequate nutrient intake are vital. In severe cases where other treatments are ineffective, surgical options such as the removal of the colon may be considered.
Lifestyle and Dietary Considerations
Adapting lifestyle and dietary habits can play a significant role in managing UC ulcerative colitis. Patients are often advised to keep a food diary to track what foods may exacerbate symptoms. Common dietary recommendations include:
- Eating smaller, more frequent meals.
- Staying hydrated by drinking plenty of fluids.
- Avoiding caffeine, alcohol, and carbonated beverages.
- Choosing low-fiber, easily digestible foods during flair-ups.
Alongside dietary changes, stress management techniques such as yoga, meditation, and regular exercise can aid in reducing the severity and frequency of symptoms. Support groups and counseling may also provide valuable emotional and psychological support for those living with UC.
Progress and Research
Ongoing research into UC ulcerative colitis continues to deepen our understanding of the disease and improve treatment methods. Advances in genetic research and biotechnology have led to the development of new therapeutic options and personalized medicine approaches. Researchers are also exploring the role of the gut microbiome in UC, which may pave the way for innovative treatments targeting gut bacteria. Clinical trials are vital in testing new drugs and interventions, offering hope for more effective management of UC in the future. By staying informed about the latest research, patients and healthcare providers can make better-informed decisions about treatment and care options.
Conclusion
Living with UC ulcerative colitis presents challenges, but with proper management and support, individuals can lead fulfilling lives. Early diagnosis, effective treatment, and lifestyle modifications are key components in managing the condition. As research continues to advance, there is optimism for even more effective therapies on the horizon. Patients are encouraged to work closely with their healthcare providers to develop a personalized plan that addresses their unique needs and improves their overall quality of life.